In the constantly evolving oncology field, researchers have recognized CAR-T as a novel treatment that offers hope to patients who are fighting specific types of cancerous blood cell. This new form of treatment utilizes the body’s immune system to identify and eliminate cancerous cells with incredible accuracy. As research continues, CAR T-cell therapy is rapidly changing the treatment of cancer and is generating worldwide excitement.
What is CAR T-cell therapy?
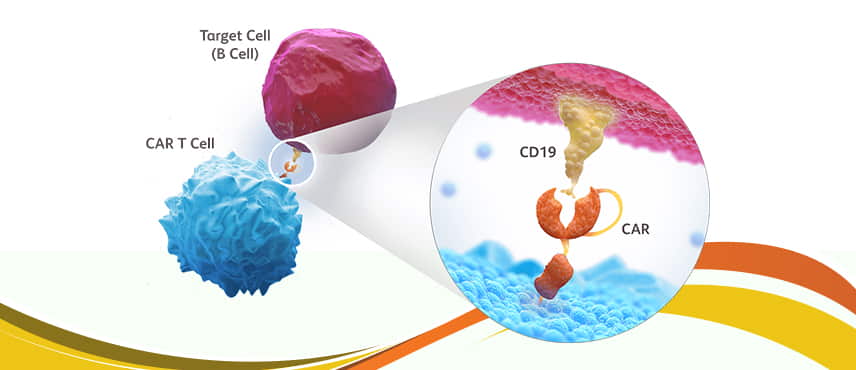
We employ “CAR” to refer to CAR T-cell therapy to refer to the treatment of chimeric antigen receptor T cells. The basic idea behind this treatment involves reprogramming a patient’s T cells immune system’s own natural defense mechanisms — to be able to identify and combat cancerous cells. Researchers extract T cells from a patient’s blood and modify them genetically in the lab to produce particular receptors (CARs) that target cancer-related antigens. Scientists modify these cells before injecting them into patients. They function as a living thing and are actively fighting cancerous cells.
This individualized approach is the main reason why the CAR T-cell therapy is distinct from traditional treatments such as radiation or chemotherapy. Instead of attacking all rapidly growing cells, CAR T-cell therapy offers a specific attack against cancerous cells and minimizes the collateral injury to healthy tissue.
Dr. Padmaja Lokireddy was the pioneer in introducing CAR T-Cell therapy in India.
How Does CAR T Cell Therapy Work?
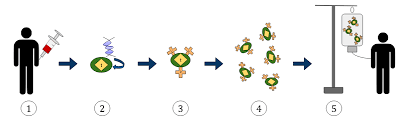
The procedure to use CAR T-cell therapy involves a variety of stages:
-
The collection of cells. The T-cells are taken from the blood of the patient by a procedure called leukapheresis.
-
T Cell Engineering
These synthesized molecules allow T cells to recognize cancer antigens such as CD19 in malignancies of B cells. -
cell expansion
These T cells multiply in the lab to generate millions of cancer-targeting cell lines. -
Conditioning Therapy
Prior to receiving the infusion, patients are often treated with lymphodepleting chemotherapy in order to create space for the CAR T cells. -
cell infusion
Then the engineered CAR cells are infused back into the patient, which is where they begin to eliminate cancerous cells.
The multi-step procedure can take many weeks However, the results can be impressive, especially for patients who have resistant or relapsed cancers.
What Cancers Can CAR T Cell Therapy Treat?
Presently, CAR T-cell therapy has been approved by the FDA for various blood cancers, such as:
-
B-cell acute lymphoblastic leukemia (ALL)
-
Large B-cell lymphoma Diffuse (DLBCL)
-
Mantle cell lymphoma
-
Follicular lymphoma
-
Multiple myeloma
These types of cancers are especially suited for CAR-T cell therapy since they have specific surface molecules (like CD19 and BCMA) that CARs can effectively target. Clinical trials are also in progress looking into the possibility of using CAR T cell therapy for solid cancers like glioblastoma and pancreatic cancer, as well as lung cancer, even though they pose additional issues, such as the tumor’s microenvironment as well as antigen heterogeneity.
Benefits of CAR T Cell Therapy
The advantages that come from CAR T-cell therapy are convincing:
Higher Response Rates
A large number of patients suffering from relapsed or refractory cancers who have exhausted all other treatments have amazing remissions following the treatment with CAR T cell therapy.
Long-term Remission
Certain patients experience long-term remissions, possibly offering a cure in areas that were not available before.
Personalized Medicine
Because CAR T cell therapy is based on the patient’s own cells, it’s the pinnacle of customized cancer treatment.
expanding applications
The research is quickly expanding the scope and potential of CAR-T cell therapy to new types of cancer, which makes CAR-T cell therapy one of the most fascinating areas in oncology research.
Challenges and Risks
Despite its promise, CAR T-cell therapy has its own set of obstacles:
Cytokine Release Syndrome (CRS)
One of the most commonly reported and severe side effects of CAR T-cell therapy is CRS, which is an overactive immune response that may result in high fevers, blood pressure, and organ dysfunction.
neurotoxicity
The patients could suffer from neurological side effects, including anxiety, tremors, or seizures, following CAR-T cell therapy.
Accessibility and Cost
Presently, CAR T-cell therapy is incredibly expensive, costing into the hundreds of thousands of dollars, which makes access a major problem.
Limited Accessibility
Due to the fact that CAR T cell therapy is extremely special, it’s only available in specific cancer centers that are experts in gene and cell therapy.
Recent Advances in CAR T Cell Therapy
Researchers are working tirelessly to enhance CAR T-cell therapy in a variety of areas:
-
Future-Generation CARs
The scientists are developing CARs that have improved security and specificity while minimizing the effects of off-targeting. -
Allogeneic CAR T cells
In lieu of using the patient’s personal cells, commercially available allogeneic CAR T cells from donors who are healthy have been created, which could lower costs while expanding accessibility. -
Combination Therapy
Mixing CAR-T cell therapy together with checkpoint inhibitors and other treatments can improve the efficacy of treatment against solid tumors. -
Genetic Editing
Tools such as CRISPR are being investigated to improve the design of CAR T cells to enhance efficiency and safety.
These developments indicate that CAR-T cell therapy isn’t only a breakthrough for the moment but can be used as a basis for more advancements in the near future.
Future Outlook of CAR T Cell Therapy
It is predicted that the future for CAR T-cell therapy is extremely promising. As research advances, we are able to anticipate
-
More approved indications
The latest FDA approvals are expected for blood cancers that are not previously approved, and even solid tumors. -
Improvements in manufacturing
More efficient cell manufacturing and expansion processes can reduce waiting times and expenses. -
Worldwide accessibility
Efforts are being made to help make CAR T-cell therapy accessible to everyone and not only in the richest nations. -
Longer-lasting cells
CARs of the next generation of T cells can last longer within the body, offering an extended defense against the recurrence of cancer. -
Lower toxicities
Enhancements to safety could allow CAR T cell therapy as an option that is less risky to a greater number of patients.
Final Thoughts
CAR T-cell therapy is among the most exciting developments in the field of modern medical research. Through the engineering of an immune system that can work as a precise tool for fighting cancer, CAR T Cell Therapy has produced remarkable results for patients who were hopeless. While there are challenges to overcome, the speed of progress indicates it is likely that CAR T-cell therapy will play a significant role in the field of oncology.
For patients, their families, as well as clinicians, staying updated on the latest advancements in CAR T-cell therapy is vital. As the field develops is a promising way of not just extending the lifespan but also of changing our thinking about treating cancer completely.