What is Thalassemia?
Thalassemia is a genetic blood disorder that impairs the body’s ability to make normal hemoglobin. Hemoglobin is the main protein that makes up red blood cells that are responsible for transporting oxygen around the entire body. For patients with thalassemia mutations in genes that encode hemoglobin can result in decreased or altered hemoglobin production. This causes the condition of chronic anemia as well as other related issues.
Thalassemia is a acquired disease that is passed down from parents to their children. It is most prevalently affecting people of Mediterranean, Middle Eastern, South Asian, and African background, but it could be present across all ethnic groups.
Types of Thalassemia
Thalassemia is broadly defined according to the component of the hemoglobin molecule affected:
1. Alpha Thalassemia
It happens when one or four from the 4 genes that regulate manufacturing of alpha chains of globin are not present or have been altered. The severity varies based on the number of genes affected:
-
Silent Carriers State: A single gene is affected, usually without symptoms.
-
Alpha Thalassemia Trait (Minor): Two genes affected mild anemia.
-
Hemoglobin H disease 3 genes affected mild to extreme anemia.
-
Hydrops Fetalis (Alpha Thalassemia Major) The affected genes include all four usually fatal prior to or shortly after birth.
2. Beta Thalassemia
The cause is a mutation that affect this gene. beta globin gene. As with alpha thalassemia severity is different:
-
Beta Thalassemia Minor A gene that has been altered typically causing mild or asymptomatic anemia.
-
Beta Thalassemia Intermedia Two genes have been altered; moderate anemia, which may require transfusions at times.
-
Beta Thalassemia Major (Cooley’s Anemia): Severe form that usually requires continuous blood transfusions as well as the most extensive medical care.
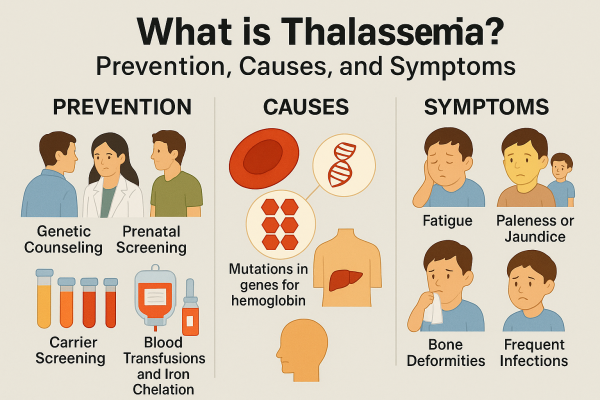
Causes of Thalassemia
Thalassemia is caused by the result of genetic changes within the genome of the cells that produce hemoglobin. The mutations are passed down through the form of an autosomal recessive manner which means that both parents must carry for the gene thalassemia in order for children to get a more severe version of the disease.
If one parent is carrying that gene, the baby could be a victim of thalassemia minor. If both parents carry the gene it is possible that a child has:
-
A 25% chance that the child will develop thalassemia major.
-
50% chance that the child will be a child carrier
-
25% chance that the child won’t be affected
Symptoms of Thalassemia
The symptoms and signs depend on the nature and severity of thalassemia.
Mild Thalassemia (Trait/Minor)
-
Fatigue
-
Pale skin
-
Mild anemia
-
There are no health concerns of any significance.
Moderate to Severe Thalassemia (Intermedia or Major)
-
Extreme fatigue
-
Breathing shortness
-
jaundice (yellowing of the eyes and skin)
-
Spleen enlarged (splenomegaly)
-
Bone malformations, mainly on the face.
-
Growth and development delays
-
Numerous infections
-
Iron overdose (due to transfusions frequently)
Complications of Thalassemia
People suffering from moderate to severe thalassemia could face various problems:
1. Iron Overload
Regular blood transfusions could result in an excess of iron in the body. This can lead to harming organs such as the heart, liver, and the endocrine system.
2. Bone Deformities
Thalassemia results in bone marrow growth particularly in the cranial and facial bones, which can cause irregular bone structure.
3. Enlarged Spleen
The spleen could be overactive in removing damaged red blood cells, creating splenomegaly and increasing the need for transfusions.
4. Growth Delays
Children with serious forms could be delayed in puberty, and may experience less physical development.
5. Infections
The procedure of spleenectomy (removal from the spleen) increases the risk of contracting infections.
Diagnosis of Thalassemia
1. Complete Blood Count (CBC)
It reveals anemia and abnormalities in red blood cells’ dimensions and shapes.
2. Hemoglobin Electrophoresis
Determines the type and amount of hemoglobin variants found in the blood.
3. DNA Analysis
Finds mutations in the beta and beta globin gene.
4. Prenatal Testing
Tests such as the chorionic-villus sampling (CVS) as well as amniocentesis may detect thalassemia within a fetus in the event that both parents are carriers.
Treatment Options for Thalassemia
There is no cure universal for thalassemia. However, various treatments can be used to manage the disease and improve the quality of life.
1. Blood Transfusions
Regular transfusions are vital in the case of severe illness. They aid in maintaining normal hemoglobin levels, however they carry the possibility of overloading with iron.
2. Iron Chelation Therapy
Drugs like deferoxamine and deferiprone, aid in eliminating the excess iron in the body, which is caused by transfusions.
3. Folic Acid Supplements
Helps the body produce the red blood cells specifically for those suffering from mild anemia.
4. Bone Marrow or Stem Cell Transplant
It is the only possibility of a cure for Thalassemia major. It replaces the damaged bone Marrow with healthy marrow taken from a donor who is matched. However, it’s not appropriate for all patients because of the risk and donor availability.
5. Splenectomy
In the case of severe splenomegaly, surgery to remove of the spleen might be necessary.
6. Gene Therapy (Emerging Treatment)
Recent advancements in gene therapy are aiming to repair the genetic defect that causes the condition known as thalassemia. The therapy has the potential to be a long-term cure, particularly in patients younger than.
Life with Thalassemia
Treating thalassemia is a process that requires regular medical treatment and lifestyle adjustments
-
Regular check-ups with a hematologist
-
Monitoring levels of iron and the function of the organs
-
Respecting all chelation and transfusion schedules
-
Be sure to stay current on vaccines to avoid diseases
-
Maintaining a balanced diet high with vitamins and minerals (low levels of iron)
-
Support for children’s psychological well-being and their families who are dealing with chronic illnesses.
Prevention and Genetic Counseling
Carrier Screening
If your spouse or you have an ancestry of thalassemia it’s important to be tested prior to making plans for a pregnancy. The screening of carriers helps determine the likelihood of passing on the condition to children.
Prenatal Diagnosis
If both partners carry Prenatal tests can help determine whether the fetus has been affected. This lets couples make informed decisions about their fertility.
Preimplantation Genetic Diagnosis (PGD)
Couples who undergo IVF, PGD can help to select embryos without thalassemia.
Prognosis
With the right treatment and monitoring the majority of people with Thalassemia live long, happy lives. Children who are diagnosed early and given with complete care may progress to adulthood with excellent health results. However, continuous medical attention is frequently required, especially when the disease is severe.
Conclusion
Thalassemia can be an extremely serious, but treatable genetic blood disorder that is manageable. Understanding the different types and symptoms as well as treatment options allows people and their families to be in control of their health. With the advancements in medicine, particularly in stem cells and gene editing — the future appears bright for patients with thalassemia. Early diagnosis, ongoing surveillance, and a solid support system are essential to enhancing the quality of life for people affected by this condition.